Palliative care
Let’s ensure people in palliative care get the assistive technology they need
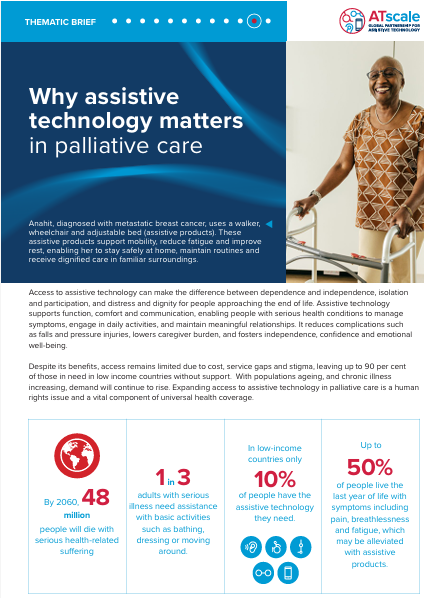
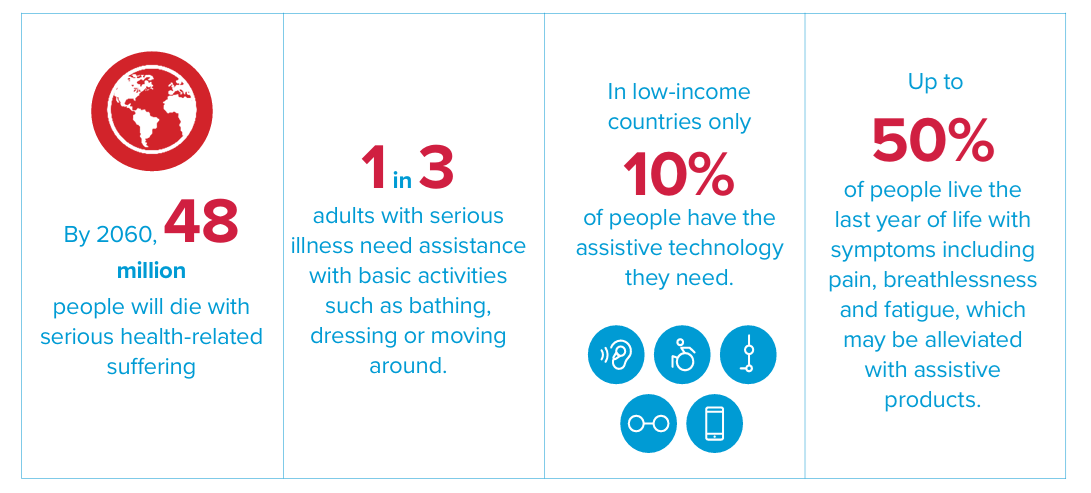
Access to assistive technology can make the difference between dependence and independence, isolation and participation, and distress and dignity for people approaching the end of life. Assistive technology supports function, comfort and communication, enabling people with serious health conditions to manage symptoms, engage in daily activities, and maintain meaningful relationships. It reduces complications such as falls and pressure injuries, lowers caregiver burden, and fosters independence, confidence and emotional well-being.
Despite its benefits, access remains limited due to cost, service gaps and stigma, leaving up to 90 per cent of those in need in low income countries without support. With populations ageing, and chronic illness increasing, demand will continue to rise. Expanding access to assistive technology in palliative care is a human rights issue and a vital component of universal health coverage.
Why assistive technology matters for palliative care
| Supports personal care, daily activities and communication, enabling people to maintain control and independence as health declines. |
| |
| Eases physical and emotional pressure on caregivers, helps families balance work and care responsibilities, and supports care in familiar environments. | ||
| Reduces preventable complications such as falls and infections, and helps manage pain, fatigue and breathlessness. | ||
| Enables participation in play, communication and family life, supporting emotional wellbeing and reducing social isolation. |
Inclusion is key to realize the Sustainable Development Goals (SDGs) and leave no one behind. There will not be full inclusion while people are unable to access assistive technology. Assistive technology cuts across all 17 SDGs and is particularly relevant to some.